-

Resource
Can you give Depo or Nexplanon on the day of a medication abortion?
Mifepristone and misoprostol are commonly used for medication abortion in the United States, up to 70 days estimated gestational age. Currently, the WHO recommends giving … <a href="https://www…July 19, 2016
-
Resource
This is How I Teach: Communication with Partial Participants in Abortion Training
Presented by, Deb Bartz Brigham and Women’s HospitalJuly 18, 2016
-
Resource
This is How I Teach: The Menstrual Cycle
Presented by: Sarah Prager, MD, MAS University of WashingtonJuly 18, 2016
-
Resource
This is How I Teach: Mastering Difficult Procedures
Presented by: Kristina Tocce University of Colorado, DenverJuly 11, 2016
-
Resource
This is How I Teach: CDC Selected Practice Recommendations
Presented by: Valerie French University of California San FranciscoJuly 11, 2016
-
Resource
Animated Uterine Aspiration Simulation Workshop
This workshop is intended to teach the steps of first-trimester abortion using an animated video of the procedure. This animation is an excellent introduction to the … <a href="https://www.inn…June 14, 2016
-
Resource
Health Disparities in Abortion and Family Planning Workshop
This workshop is intended to teach about differences in abortion rates across racial and socioeconomic groups. Workshop Objectives: At the end of the workshop, learns will: … <a href="https://…June 13, 2016
-
Resource
Incorporating Partial Participants in Abortion Training
Presented by: Deborah Bartz, MD, MPH Harvard UniversityJune 8, 2016
-
Resource
Abortion after the First Trimester
Facilitator Guide with Quiz Learning Objectives: By the end of the session, learners will be able to: State the proportion of abortions that take place … <a href="https://www.innovating-educati…May 13, 2016
-
Resource
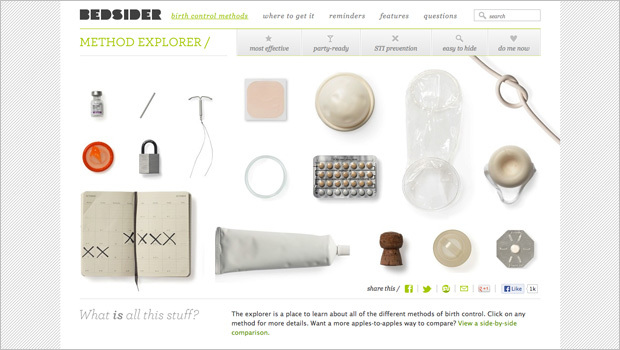
Using Bedsider As a Teaching Tool with Medical Students
Many clinicians use Bedsider to help patients decide which method of contraception best fits their lifestyle. Bedsider is a free birth control support network that … <a href="https://www.innova…April 25, 2016
Sort
Filter by Type
Filter by Topic