-
-

Resource
Improving Contraceptive Counseling through a Shared Decision Making Approach: A New Medical Curriculum
Family planning providers can help women choose a contraceptive method that is the best fit for their preferences, lifestyle and reproductive goals. Shared Decision Making … <a href="https://ww…April 20, 2016
-

Resource
LGBTQ Health Resources for Medical Educators
Many of our LGBTQ patients experience unique challenges and barriers to accessing high-quality, patient-centered health care services. The historical disparities in the care they have … <a href…April 6, 2016
-
Resource
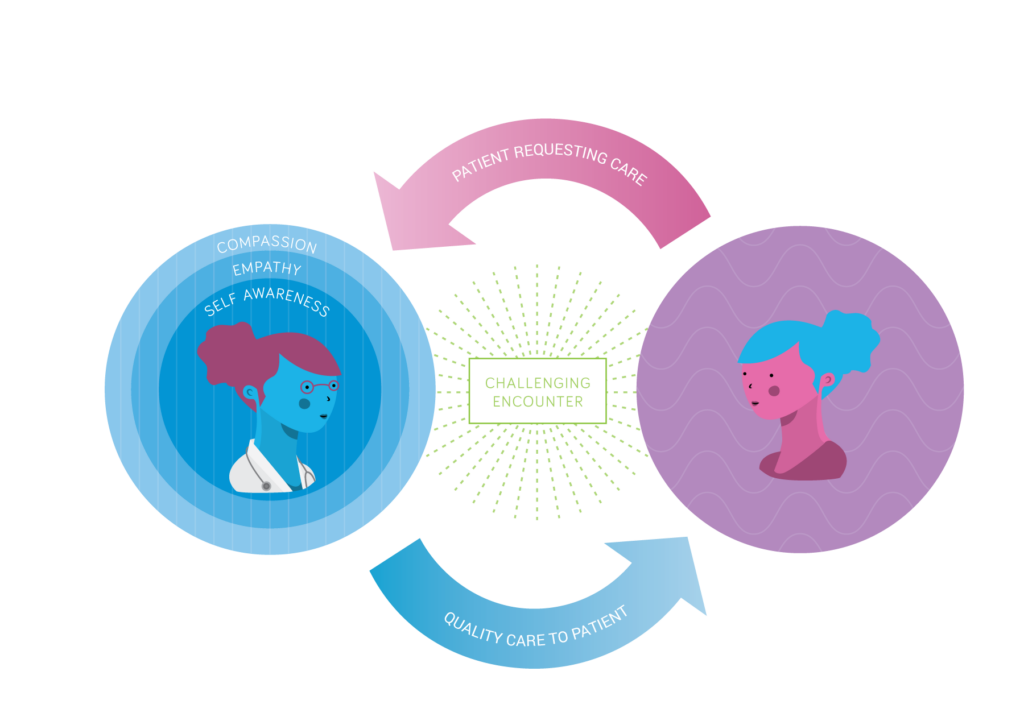
Caring For Challenging Patients Digital Module
This web-based Caring for Challenging Patients workshop is intended to help learners develop skills to manage their own judgmental feelings in patient interactions by encouraging empathy, … <a…April 5, 2016
-

Resource
Changing the Conversation: Shared Decision-Making in Reproductive Health
The process of shared decision-making (SDM) requires clinicians to set aside their personal biases or preferences for care, offer balanced information about all treatment options, … <a href="ht…April 4, 2016
-
Resource
Innovative Resident Education: Digital Learning
Having enrolled in the recent video course Abortion: Quality Care and Public Health Implications I came away from the experience impressed and more educated. After more than … <a href="http…April 1, 2016
-
Resource
All Materials: Abortion Training for Partially Participating Residents
Download all materials for the Abortion Training for Partially Participating Residents using the links below. Partial Participation Protocols ACOG Committee Opinion on Abortion Training ACOG Committe…April 1, 2016
-
Resource
Immediate Postpartum Intrauterine Device Insertion Training Workshop
This workshop is intended to teach the steps of postpartum IUD insertion. Lisa Goldthwaite, MD, MPH Stanford University Kristina Tocce, MD, MPH University of Colorado … <a href="https://www.inn…March 29, 2016
-
-
Resource
Caring For Challenging Patients Workshop
Teaching Patient-Centered Care At the core of professionalism is the recognition that patient-centered care is the foundation of positive health outcomes. Patient-centered care challenges doctors &hel…March 18, 2016
Sort
Filter by Type
Filter by Topic